By Alfred Poor, The Health Tech Futurist
In the past decade, health technology has raced ahead at an unprecedented pace. We are seeing new tools that help diagnose and treat a wide range of illness and chronic disease sooner and more effectively. Telemedicine brings healthcare services to those who need it but who have difficulty getting to a hospital or other clinical setting. Remote patient monitoring can detect problems before they become emergencies requiring an ambulance ride and an expensive hospital readmission.
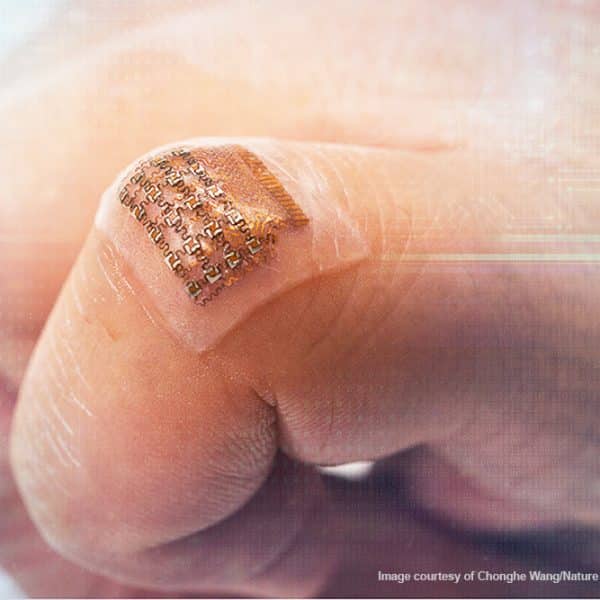
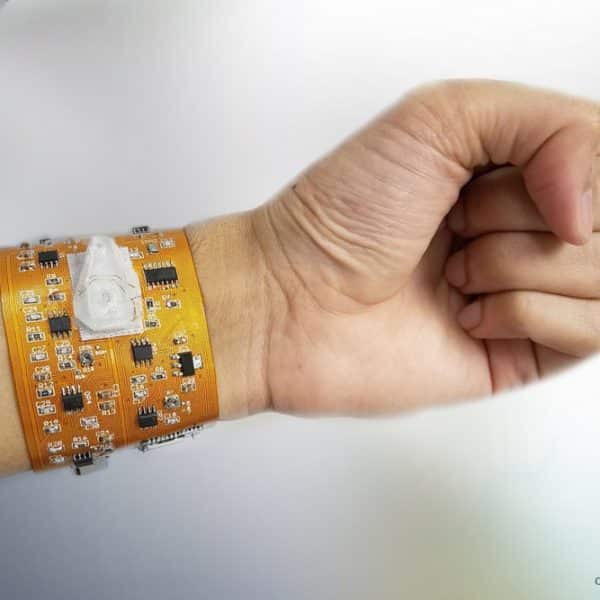
New wearables make it possible to automatically maintain a diabetic patient’s blood glucose levels within a much tighter range, greatly reducing the chance of expensive and life-changing secondary complications such as blindness or the loss of a limb. Smart implants can monitor important biometrics such as glucose levels without the frequent need for invasive finger sticks to draw blood. Innovation is not limited to diabetes. Exoskeletons and smart prosthetics can reduce healthcare costs while delivering a better quality of life. The list of disruptive innovations is nearly endless. But almost all of them share a common challenge; I call it the “Left-Pocket/Right-Pocket Problem.” A 2009 program in Camden, New Jersey, serves as a poster child demonstration of this situation. According to one government report, about half of all Medicare expenditures are spent on just five percent of the eligible beneficiaries. In Camden, a consortium of city hospitals pooled their data and discovered that one percent of the patients visiting the hospitals were responsible for $46 million in treatment costs over a five-year period.
A pilot program put together a team that targeted just 35 of these “frequent flyer” patients who racked up an average $1.2 million in hospital charges per month. Social workers coordinated their healthcare and other aspects of their lives, such as getting into drug treatment programs. They provided housing for the homeless patients and saw that they ate balanced meals every day. The result? The average monthly hospital costs were cut in half to $531,000. The cost of the program for a year was about $300,000. That amounts to a 20:1 return on investment. Here’s the problem; I don’t know of many hospital emergency departments that have line items in their budgets that cover apartment rent and social workers for homeless patients. The expenses come out of the left pocket, but the savings go into the right pocket. (Or to be more accurate, the “savings” mean that less money is taken out of the right pocket.) This is the challenge for disruptive health tech. It’s not enough to solve a problem; there must be a sustainable business model that pays for the new technology so that its development and production are sustainable.
Diabetes costs more than $300 billion each year in the U.S. alone, including both healthcare costs and reduced productivity. Imagine if a closed-loop wearable system could cut those costs by just one third, by eliminating many of the instances of costly complications. $100 billion is enough to pay more than $3,000 per year to each person with diabetes in the U.S. That would be more then enough to pay for a closed-loop insulin pump system for each patient. Similar cases can be made for other chronic diseases and ways that wearable health tech devices can provide a significant return on investment: COPD, heart failure, various forms of vision impairment, and more.
The problem is that we don’t have a closed-loop financial system to support these innovations. The savings – or reduced costs – benefit one entity’s budget while the cost of such programs might have to come from some other source.
We are seeing some signs of hope, however. For example, the Veterans Administration is a much more self-contained entity than some other healthcare organizations. The VA has been able to undertake some landmark projects in telehealth, especially in the areas of mental health treatment. The result has been greatly improved outcomes at much lower costs.
Businesses are another example of where health tech disruption is gaining traction. Employee fitness incentive programs have been proven over and over to have a real and significant return on investment that can transfer directly to a company’s bottom line. In addition to controlling healthcare costs (either direct costs or insurance premiums), these programs have been shown to reduce absenteeism, increase productivity, foster employee engagement, and improve employee retention. These gains can add millions of dollars to a business balance sheet every year.
While it’s important to build a better mousetrap, the world won’t beat a path to your door if you don’t have a way to pay for it. Health tech businesses must do more than just show that their products and services will save money; they must also show how the money can move through the system to cover the costs of the devices in the first place.
Author bio: Alfred Poor, the Health Tech Futurist, believes that innovative health tech will save healthcare in the U.S. and worldwide by lowering costs and improving outcomes. He is a full-time technology speaker and writer, and is the Editor of Health Tech Insider, an industry website and newsletter that covers wearable and mobile devices for health and medical applications.